Abby Lorion ’25 and Charlotte Kloman ’25 - Beth Israel Lahey in Wayland, MA
- The Rivers School

- Aug 5, 2024
- 5 min read

Over the course of a two-week period, we had the privilege of shadowing Dr. Deborah Riester, who specializes in Internal Medicine and Endocrinology at Beth Israel Lahey in Wayland, MA. While we observed many patients living with prediabetes, type 1 and type 2 diabetes, we also saw a variety of other cases, including varying levels of osteoporosis, mast cell activation syndrome, hypertension, hyperparathyroidism, and potential cases of tick-borne diseases such as anaplasmosis and ehrlichiosis. After shadowing Dr. Riester, we would then research conditions, medications, mechanisms of medications, as well as their side effects, and report our findings to her.
We had the opportunity to work with the rest of Dr. Riester’s team (Christina, and Carly) as well. We saw a case with microalbuminuria (proteins in her urine that indicate potential kidney failure, which Dr. Riester was trying to prevent). We learned about DKA in Type 1 diabetics (diabetic ketoacidosis: a complication of diabetes that occurs when the body produces high levels of blood acids called ketones). And we watched a finger stick and EKG being administered to a pre-op patient, as well as several a1c and lipid level labs being run. We spent time learning how to feel for abnormal thyroids using a swallow test and proper hand placement. A rare case of mast cell activation syndrome came in for his physical, showing signs of malnourishment due to a two-food diet that is tolerated by his condition, which causes the sensation of an allergic reaction despite not being allergic to the ingested product. We also saw the mental health side of diabetic care, witnessing how patients are unable and unmotivated to care for themselves due to external factors in their personal lives and the impact that their condition has on them.
Computer setup for research Basic exam room for patients Restocking gloves
One of the first things we learned about was the A1c test. An A1c test, also known as a hemoglobin A1c test, is a blood test that measures your average blood sugar levels over the past two to three months. It is used to diagnose and monitor diabetes. The test provides valuable information about how well your blood sugar levels have been controlled over time. A higher A1c level indicates poorer blood sugar control, while a lower A1c level indicates good control. A high A1c (over 6.4%) signifies a patient is diabetic; an A1c between 5.7% and 6.4% suggests pre-diabetes which concludes that an A1c under 5.7% implies that the patient is not diabetic.
The EKG can be used in many different circumstances, but we primarily saw it used for pre-op patients. An electrocardiogram is a test that records the electrical activity of the heart. It is used to detect and diagnose heart problems such as abnormal heart rhythms, and coronary heart disease. Identifying any underlying heart conditions is imperative as they could pose a massive threat to surgery, and so administering this test allows for a quick and safe procedure and recovery.
Prior to seeing Dr. Riester, every patient who came into the office got their blood pressure. Blood pressure is depicted as two numbers: xxx/xx. The top number is the systolic pressure, which is the pressure of the blood on the artery walls while the heart is pumping. The bottom number is the diastolic pressure, which is the pressure of the blood on the artery walls when the heart muscles are relaxed between beats. <120/80 is normal, 120-129/<80 is elevated, 130-139/80-89 is symptomatic of hypertension (high blood pressure), and >140/90 is considered stage two hypertension.
Ozempic: Ozempic acts on GLP-1 receptors in the hypothalamus (the brain region involved in appetite regulation), and by activating the receptors, it reduces hunger and leads to decreased food intake. Ozempic can cross the blood-brain barrier, which allows it to exert its effects directly on the central nervous system, which is crucial for its ability to influence appetite and food intake. It also slows the rate at which food leaves the stomach to cause a further feeling of fullness and reduces food intake to aid in weight loss.
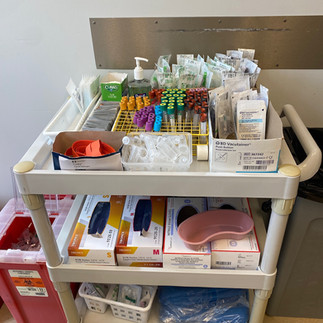
Phlebotomy supply cart in lab Basic examination tools A1c and lipid count machines use blood samples
Metformin is the “first line” treatment for diabetes, and it works by decreasing the amount of glucose your body absorbs from things ingested, reducing the amount of glucose that the liver makes, and helping the body’s natural insulin to work better. Insulin is a hormone that helps your body use glucose as a source of energy. Common side effects are gastrointestinally related.
Jardiance is Dr. Riester’s second choice of treatment if the patient is not tolerating Metformin. Used to lower blood sugar levels in people with type 2 diabetes. It is indicated to reduce the risk of cardiovascular death, renal failure, and heart attacks in adults with type 2 diabetes and established cardiovascular disease. It can also be used to treat heart failure with a reduced ejection fraction. Jardiance works by inhibiting the SGLT2 protein in the kidneys, which helps remove glucose from the body through urine. Doing so helps lower blood sugar levels and provides cardiovascular benefits by reducing the risk of heart-related complications.
On-site lab Charlotte doing research while Standards of Care Pamphlet
Abby sees a patient
Motivational Interviewing:
Our “motivational” questions:
Where do you see yourself a year from now? What is a change you could make to get closer to that version of yourself?
What is something about your condition/diagnosis/diabetes that you want to be in control of?
What forms of reminders would be helpful for you to maintain and manage your daily health?
Dr Riester’s “instructional” suggestions
Develop a healthier diet
Increase exercise
Check blood sugars often
The project that we completed while working with Dr. Riester was comparing the results of motivational interviewing to more conventional and instructional interviewing. The motivational questions are supposed to give the patient a chance to self-identify areas that could warrant improvement, and prompt them to find solutions that they believe will be helpful and tailored best to them. The instructional interviewing is when Dr. Riester simply tells them what they need to be doing in order to see improvements in their condition. We were curious to see if the motivational interviewing allowed patients to have a sense of control and gave them the drive to take care of themselves, as opposed to simply being told what they needed to do. We questioned a total of eight patients— three were asked the conventional questions and the other five were asked the motivational questions.
Instructional Interviewing
| Motivational Interviewing
|
After following up with the patients about a week later, these were our findings:
Motivational patients were more likely to move forward with the small improvements that they identified themselves rather than being directly told what to do.
A patient who was initially in the instructional category automatically began self-motivating and had his own ideas on how to improve.
In observing the interviews, we noticed that patients with higher A1c levels were less compliant and less likely to change their habits to lower their A1c, presumably because it seemed like a larger and bigger task to undertake, no matter how they were interviewed.
Finally, we would like to say a huge thank you to Dr. Riester for allowing us to observe her helping countless patients and teaching us about their conditions in this medical field. Furthermore, a huge thank you to her staff, patients, and Mr. Schlenker for providing us with the opportunity to experience endocrinological health care up close!




















Comments